Research Overview
We are broadly interested in the discovery, functional analysis, and therapeutic targeting of genes that are altered in human disease. We seek to understand how different types of genetic changes affect the function of human genes and influence the molecular phenotype within a single cell. By understanding the underlying function of a genetic mutation at its fundamental level, we can identify potential targeted therapies for a wide variety of clinical diseases.
Our research lab leverages genomic tools to understand how both rare and common human genetic variation contribute to and cause human disease. As the sequencing technology has matured, one of the major challenges in genomics is interpreting the majority of the DNA base pairs that are sequenced within an individual -- an important next step in integration of research findings into the clinical setting.
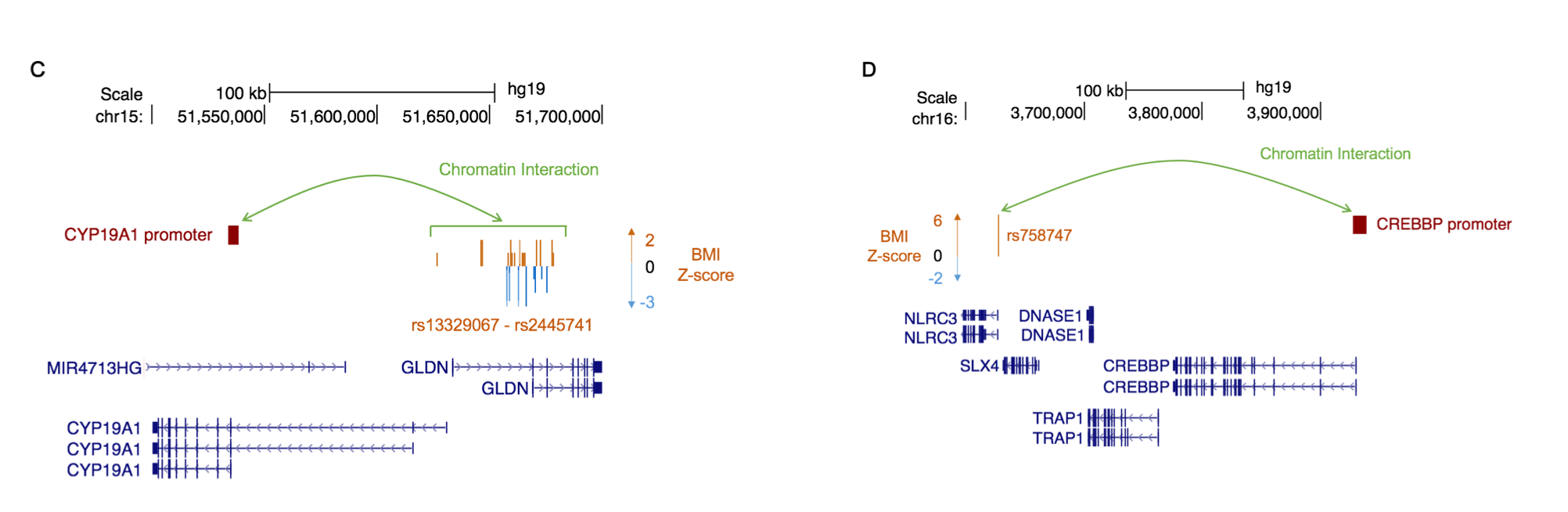
The lab takes a bidirectional approach. First, we are interested in rare genetic syndromes caused by genetic changes in genes that function to organize DNA through chromatin modification. The lab leverages functional genomic approaches (RNA-seq, ChIP-seq, methylation-seq, CLIP-seq, and Hi-C) to 1) understand how rare deleterious mutations in chromatin modifiers affect downstream pathways and human development in a cellular model system, 2) identify modifiers of disease severity, and 3) prioritize putative drug targets. Second, we are also interested in the shared genetic basis of monogenic and complex diseases. We are using existing large scale GWAS data sets to better identify and interpret findings by leveraging the extremes of the phenotypic spectrum (monogenic/Mendelian disease).
Our current focus is on genetic syndromes that are due to rare pathogenic mutations in genes that are important for chromatin conformation (a.k.a. chromatin modifiers).